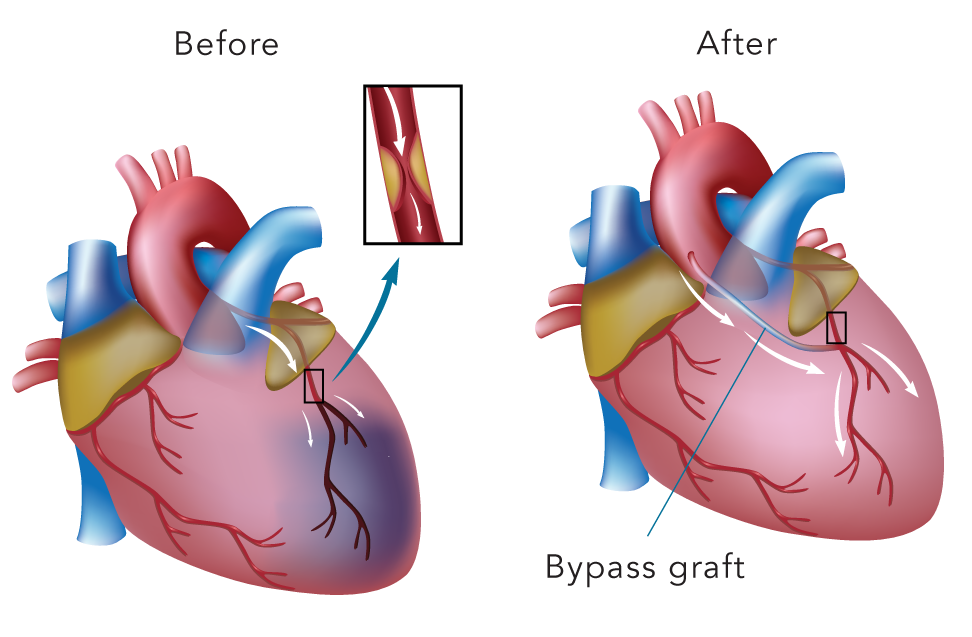
Coronary Artery Bypass Grafting (CABG) is a surgical procedure that improves blood flow to the heart muscle. It entails diverting the flow of blood around a section of a blocked or partially blocked artery by creating new pathways to the heart muscle, hence the term bypass. During coronary bypass surgery, a healthy blood vessel is taken from the patient’s leg, arm or chest to create a new pathway so that blood bypasses the diverted or blocked area.
CABG is the most common type of open heart surgery in many countries. It is a lifesaving surgery that can help improve the quality of life and improve longevity in certain subsets of people with coronary artery disease. However, it is still important to lead a healthy lifestyle to ensure the effectiveness of the procedure is sustained.
- The patient has chest discomfort or breathlessness caused by the narrowing of several of the arteries that supply one’s heart muscle. Sometimes, angioplasty and stenting will help, but for some types of blockage, coronary bypass surgery may be a better option.
- The patient has more than one coronary artery disease and the function of the heart muscle is impaired.
- The patient’s left main coronary artery is severely narrowed or blocked. This artery supplies most of the blood to the left ventricle, the main pumping chamber of the heart.
- Improves the quality of life
- Improves longevity in certain subsets of patients
- Improves the heart function, thereby, decreasing the risk of a future heart attack
- Increases chances of surviving a future heart attack
Today, the majority of people who undergo CABG have an 80% to 90% chance of having no symptoms of heart disease for at least 10 years.

The risk of developing complications is generally low. Any risks of complications will be discussed individually with patients by the surgeon prior to surgery
After CABG, patients are recommended to join a cardiac rehab programme. It is a customised programme of exercise and education, which often begins while they are still in the hospital. Patients may continue the rehabilitation programme in the outpatient setting.

While at home, patients are advised to do light exercise but avoid extreme physical activity for at least 4 to 6 weeks. The patients will see the doctor a week after the surgery and then a month later. Subsequently, patients will be seen regularly every six months. ECGs and blood work out are routinely done in the outpatient follow-up. After 6 to 8 weeks after the surgery, patients can resume their driving. Depending on the type of work, one may be able to perform light work in the office after 8 weeks.